The health information exchange(HIE) between patients and healthcare providers(HPs) is a cornerstone of the digital transformation of healthcare and a critical enabler for co-creating health value. In the framework of health value co-creation theory, HIE-based medical services can be divided into four categories on the basis of the degree of patients and HPs’ participation[1]: The first service mode is the traditional medical model(TMM), which is a base data storage between patients and HPs[2], such as the electronic health record. The second service mode is collaborative care(CC), which is originally designed for interoperability and knowledge sharing among HPs[3]. The third service mode is self-managed care(SMC), where patients exert effort to report information to help HP monitoring and predict health status. The last service mode is healthcare value co-creation(HVC), where patients and HPs are co-creators with medical information[4] and jointly contribute to healthcare delivery efficiency and treatment outcome. Studies show that HIE saves 1 298 US dollar per procedure by reducing the length of stay by 30% and reducing preventable 30-day readmission by 38.2% for a hospital[5].
HIE sustainability and operational maturity are always considered as serious obstacles in spite of the existence of numerous business models[6]. The longevity of HIE is excessively dependent on government investment or external funding[7]. Specifically, the Coronavirus disease 2019 allowed telemedicine to flourish; more than 50% of medical visits were conducted via HIE at the height of the pandemic; however, the significant decline in user participation at the end once again highlighted the problem of HIE sustainability[8]. Therefore, our work aims to analyze how to achieve the sustainability of healthcare information services under patient—HP co-creation.
We build a three-party healthcare supply chain that includes the HIE platform, HPs, and patients within an evolutionary game structure. We also construct mathematical models of the participant evolutionary process under four service modes(i.e., TMM, CC, SMC, and HVC). In addition, we conduct a numerical simulation to investigate the impact of service upgrading on HIE platform sustainability as an extension.
Compared with most research that uses static game theory to analyze HIE sustainability, our work uses the evolutionary game method, which allows us to understand how co-creators’ trivial actions under different dynamic service modes can trigger deviation from equilibrium, such as initial participation ratio and information quality. Given that this method has the advantage of capturing the group decision interaction process, it is widely used in the study of information service platform sustainability[9-11]. We differ from previous studies because we define patients as co-creators who shape treatment outcomes. In previous studies, patients are defined as consumers, and treatment outcomes are solely dependent on care providers’ judgment. In sum, our work emphasizes patients’ role in co-creating value for medical information services, as opposed to recipients of service prices in previous research on patient engagement[12-13]. Moreover, we define HIE sustainability as the user(patient and HP) constant engagement in a value-based healthcare delivery setting, which differs from existing studies where HIE sustainability is equal to HP profitability[2,14-15].
1 Model
To explore the effect of interaction between patients and HPs on the HIE platform, we consider a healthcare service supply chain constructed by a group of HPs, a group of patients, and one HIE platform. Patient i has a binary decision on their effort for health data sharing. The λ fraction of the patient’s invested high compliance belongs to group PH with effort cost ![]() The higher the compliance, the more the information quality of the patient increases, which benefits co-creation and health value [16], such as improving doctors’ understanding of physical conditions by providing more ample information. Therefore,
The higher the compliance, the more the information quality of the patient increases, which benefits co-creation and health value [16], such as improving doctors’ understanding of physical conditions by providing more ample information. Therefore, ![]() is denoted as self-management effect to represent the quality of patient information sharing, where a is the quality ecoefficiency of effort. Accordingly, a 1-λ fraction of a patient has low compliance categorized as group PN with effort cost
is denoted as self-management effect to represent the quality of patient information sharing, where a is the quality ecoefficiency of effort. Accordingly, a 1-λ fraction of a patient has low compliance categorized as group PN with effort cost ![]()
In general, HPs invest in basic or advanced levels of information exchange service[14]. For HP j, we have μ possibility with advanced service grouped HH with cost ![]() The advanced information service provides a knowledge effect for treatment; for example, communication with others allows HPs to keep up to date on the latest knowledge in medicine and technology, and physicians can choose better or safer treatments for patients[17]. The knowledge effect is correlated to the number of HPs in the network. HP information quality is denoted by μqH where qH is quality. A 1-μ fraction of HPs’ non-advanced service exists, which is denoted as HN with cost
The advanced information service provides a knowledge effect for treatment; for example, communication with others allows HPs to keep up to date on the latest knowledge in medicine and technology, and physicians can choose better or safer treatments for patients[17]. The knowledge effect is correlated to the number of HPs in the network. HP information quality is denoted by μqH where qH is quality. A 1-μ fraction of HPs’ non-advanced service exists, which is denoted as HN with cost ![]() Meanwhile, the basic information service provides an operational effectiveness effect represented by α, such as reduced HP costs as fewer duplicate tests, office consumables, and fewer health records.
Meanwhile, the basic information service provides an operational effectiveness effect represented by α, such as reduced HP costs as fewer duplicate tests, office consumables, and fewer health records.
We define co-create factors βij∈(0,1) to distinguish between the utility of value co-creation of different service modes, which include operational efficiency effect, knowledge effect, and self-management effect. In TMM mode, where patients provide low-quality information and HPs invest in basic information service, only basic data connectivity can be achieved, hence it is an efficiency impact. The CC mode, where HPs invest in advanced information sharing services, provides HPs with access to medical knowledge to aid auxiliary diagnosis. Thus, it has a knowledge effect. The SMC mode, where patients must exert more effort to self-report, helps HPs send direct feedback to patients. Therefore, it has an efficient and self-managing effect. HVC, where high patient compliance and HP investment are excluded, consists of intelligent diagnosis and treatment based on patient self-reports and existing medical knowledge. Hence, it has a knowledge and self-management impact. The initial health condition for patient i is ![]() and the decline rate without HP treatment is ε(0<ε<1); the decline rate for patient i, after being treated by HP j denoted as εij∈(0,1), is convex decreasing with co-created factors βij; that is, the co-creation effect decreases health value slowly if it is positive[18], and the reduction of deterioration becomes increasingly
and the decline rate without HP treatment is ε(0<ε<1); the decline rate for patient i, after being treated by HP j denoted as εij∈(0,1), is convex decreasing with co-created factors βij; that is, the co-creation effect decreases health value slowly if it is positive[18], and the reduction of deterioration becomes increasingly ![]() We assume that the function of decline is εij=εe-βij for brevity. To compare the four service models, we use the difference between the deterioration of health value before and after intervention as a proxy index for improvement in health value, denoted as
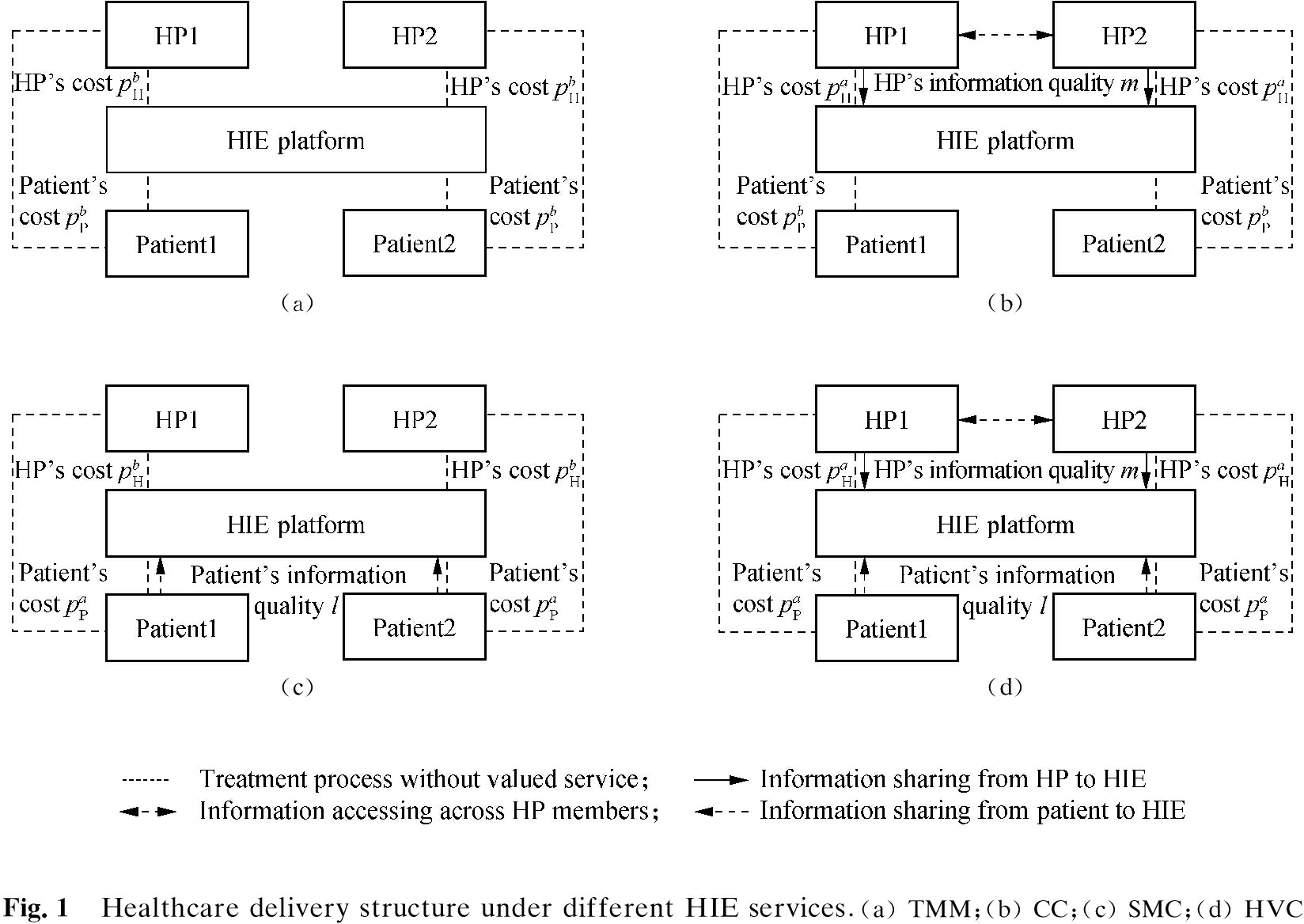
We assume that the function of decline is εij=εe-βij for brevity. To compare the four service models, we use the difference between the deterioration of health value before and after intervention as a proxy index for improvement in health value, denoted as ![]() Without losing generality, we assume that patients’ perceived benefit is constituted by health value and medical cost. Fig.1 illustrates four different medical service chains on the basis of various services in the HIE platform. Tab.1 shows the payoff matrices of patients and HPs under different service strategies.
Without losing generality, we assume that patients’ perceived benefit is constituted by health value and medical cost. Fig.1 illustrates four different medical service chains on the basis of various services in the HIE platform. Tab.1 shows the payoff matrices of patients and HPs under different service strategies.
Tab.1 Payoff matrices of patients and HPs
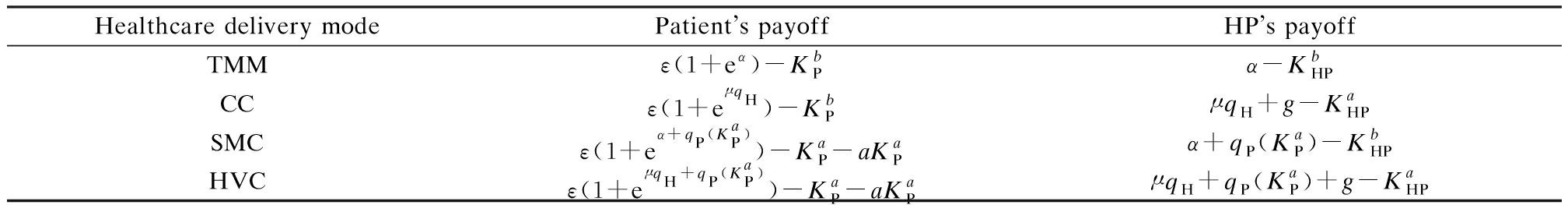
Healthcare delivery modePatients payoffHPs payoffTMMε(1+eα)-KbPα-KbHPCCε(1+eμqH)-KbPμqH+g-KaHPSMCε(1+eα+qP(KaP))-KaP-aKaPα+qP(KaP)-KbHPHVCε(1+eμqH+qP(KaP))-KaP-aKaPμqH+qP(KaP)+g-KaHP
The efficacy of patients with high compliance is calculated as follows:
(1)
Meanwhile, the benefit of patients with no compliance is equal to
(2)
Hence, we can obtain the mixed strategy expectations of patients as follows:
uP=λμε(eμqH+qP(c)-eμqH)+λ(1-μ)ε(eα+qP(c)-eα)-
(3)
Similarly,HPs with a high investment in advanced information service can be represented by
(4)
In contrast, HPs with low investment can obtain
(5)
The benefit for all HPs can be represented as
(6)
2 Equilibrium Analysis
The participation of patients and HPs in the HIE service platform changes dynamically according to their expected utility. By analyzing the existence and location of the evolutionary equilibrium solution, we have an insight into whether the HIE platform is sustainable. We solve the evolutionary stability strategy on the basis of the replication dynamics of the choice of HPs and patients. For patients, we have the replication dynamics below:
(7)
The second derivative formula is
(8)
A cooperation-driven patient has two boundary equilibrium points 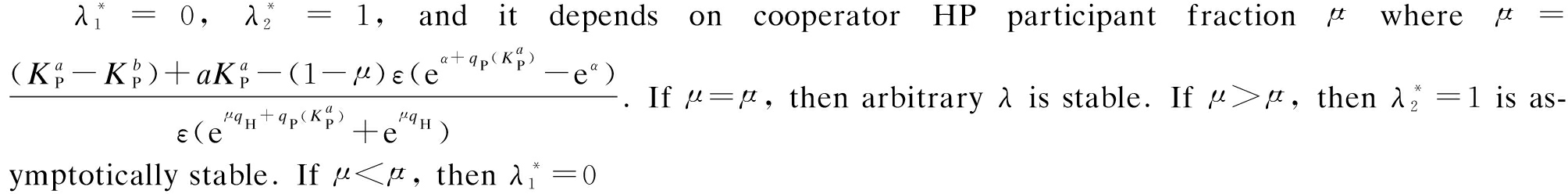 is asymptotically stable.
is asymptotically stable.
Patients’ final group decision depends on cooperator HPs’ group participant level, which is a threshold denoted as ![]() a unique optimal participant level for the patient group exists. When the HP participant level is relatively lower than
a unique optimal participant level for the patient group exists. When the HP participant level is relatively lower than ![]() patients are encouraged to share data and their final optimal group decision for them to participate in HIE. The proof is omitted.
patients are encouraged to share data and their final optimal group decision for them to participate in HIE. The proof is omitted.
For HPs, we have the replication dynamics below:
(9)
The second derivative formula is
μ(1-μ)qH
(10)
The upgrading-driven HP has two boundary equilibrium points: 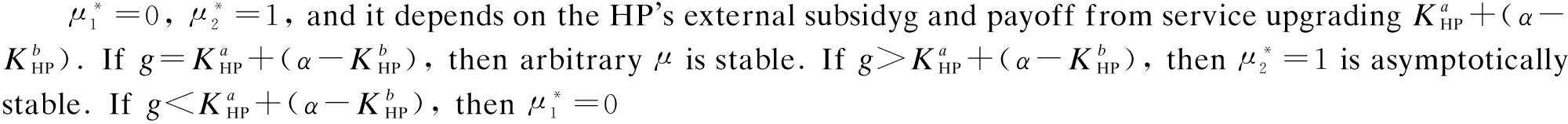 is asymptotically stable.
is asymptotically stable.
Different from patients’ group decision that relies on cooperators’ decision, we can see that HPs’ optimal decision only depends on external subsidy and payoff from service upgrading. When external subsidy counteracts the cost for service upgrading, HPs have no difference in sharing data and maintain the status quo. When the external subsidy is higher than the cost for service upgrading, the group decision for HPs is to participate in HIE. On the contrary, no HP is willing to share when the external subsidy is lower than the cost for service upgrading. The proof is omitted.
3 Numerical Simulation
From the previous analysis, we summarize that the motivation for patients to join HIE comes from cooperation, whereas that for HPs comes from service updating. To effectively enhance the HIE sustainability and the cooperation between patients and HPs, a simulation experiment is conducted to analyze the effect of the initial state of population and information quality on the system sustainability. Moreover, the effect of implementing a new payoff for either patients or HPs on platform sustainability is explored.
3.1 Sustainability
We assume that the quality of patients and HPs information is divided into three levels(low, medium, and high). Thus, a 3×3 state matrix unveils all combinations for the choices of both sides. In each combination, we set that the initial proportion of patients and HPs actively participating in HIE is 0, which increases to 1 with a step size of 0.01 to go through a total of 100 × 100 initial scenarios. During the whole five periods, we output the payoff of patients and HPs at each time point; specifically, the numerical values of the different levels of information quality for HP qH⊆[2,5,10] and patient information quality qp⊆[0.2,0.5,0.8]. We calculate the sum of the utility of patients and HPs that represents the stationary value of HIE sustainability, which is defined according to the following equation:
〈s〉![]()
(11)
The thermodynamic diagram(see Fig.2) demonstrates that the payoff evolution process is plotted in each subgraph according to the different data quality levels of both parties. Different patient information quality levels(low in the left column, medium in the central column, high in the right column) and different HP information quality levels(low in the top row, medium in the central row, high in the bottom row) are also presented. The left column pictures show the interaction of a patient and an HP when the patient information quality is relatively low. The medium column offers the result when the patient information quality is intermediate, whereas the right column presents high-quality patient information. Correspondingly, longitudinal comparisons can yield insights into different HP information quality scenarios. The abscissa in each subgraph represents the proportion of patients participating in data sharing in the initial stage, whereas the ordinate represents the proportion of HPs with advanced service in the initial stage. We show the 〈s〉 value(with color) to distinguish the overall sustainability of the platform in evolution and the convergence in each scenario. The “purple” part indicates the highest value of sustainability 〈s〉, whereas the “red” part represents the lowest value.

Platform sustainability is closely related to patient self-management compliance in terms of the quality and quantity of patient data shared. Fig.5 shows that, except for low HP information quality, a high percentage of patient engagement always achieves the highest level of platform sustainability. In general, the lowest sustainability only occurs when patient information quality is low(in the right column). Therefore, patient information quality is the key to improve the total utility of the HIE platform.
3.2 Service updating
The HIE platform has insight and conducts price adjustments to maintain sustainability during operation. We introduce service updating in the simulation to analyze the feedback of HIE platform users on their utility changes.
In the first stage,following Babu and Mohan’s[11] research, we consider four types of payoff provided by the HIE platform to manage the sustainability for patients and HPs: Undesirable(U), Feasible-1(F1), Feasible-2(F2), and Best(B)(see Tab.2). When the patient payoff is U, the benefit of data sharing or advanced information exchange service is low. Hence, patients are unmotivated to provide more quality health data. When the payoff is Feasible, whether patients can avail of advanced service within or outside the HIE platform is undetermined. When the payoff is B, patients can use the advanced service provided by HIE. The same holds for HPs in terms of information sharing quality. In the second stage, we consider that the platform will provide an opportunity for consumers and healthcare institutions to update or maintain their current service. To simplify the analysis, we ignore the situation when consumers and institutions terminate services, which means the payoff type in the second stage ought not to lead to worse than the current payoff, regardless if it is for consumers or HPs.
Tab.2 Payoffs for service update and initial participant state
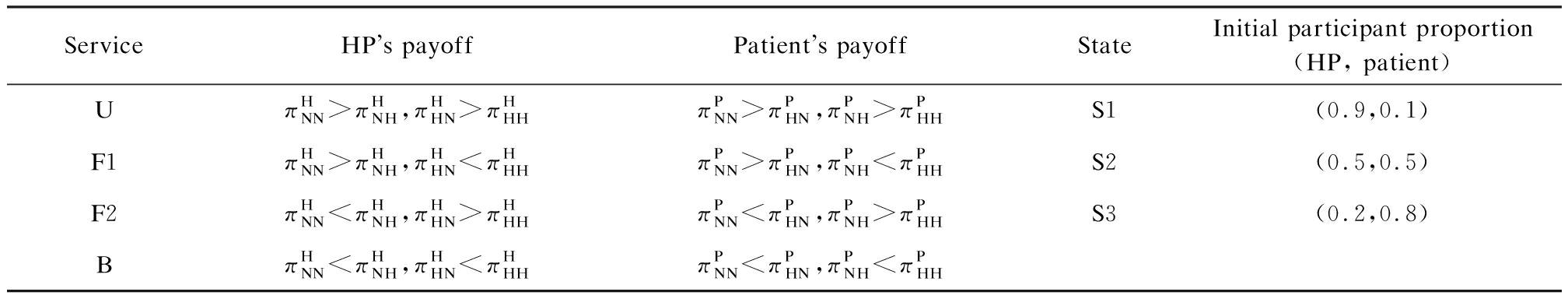
ServiceHPs payoffPatients payoffStateInitial participant proportion(HP, patient)UπHNN>πHNH,πHHN>πHHHπPNN>πPHN,πPNH>πPHHS1(0.9,0.1)F1πHNN>πHNH,πHHN<πHHHπPNN>πPHN,πPNH<πPHHS2(0.5,0.5)F2πHNN<πHNH,πHHN>πHHHπPNN<πPHN,πPNH>πPHHS3(0.2,0.8)BπHNN<πHNH,πHHN<πHHHπPNN<πPHN,πPNH<πPHH
For this question, the specific experiment is set up as follows: We first trace the dynamic process for ten periods. Then, we change the initial payoff of either patients or HPs in the middle procedure(period 5) and simplify the initial engaging of two groups of HIE users into three scenarios: S1, S2, and S3. We take the example of HP state S1=[0.9, 0.1], which indicates that 90% of HPs invest low in HIE service, whereas only 10% purchase high in HIE service. According to the initial participation status(S1, S2, and S3), sharing information quality(low, medium, and high), user pre-payoff type, and user post payoff type(U, F1, F2, and B), we tag each experiment and finally obtain valid results from 236 experiment settings.
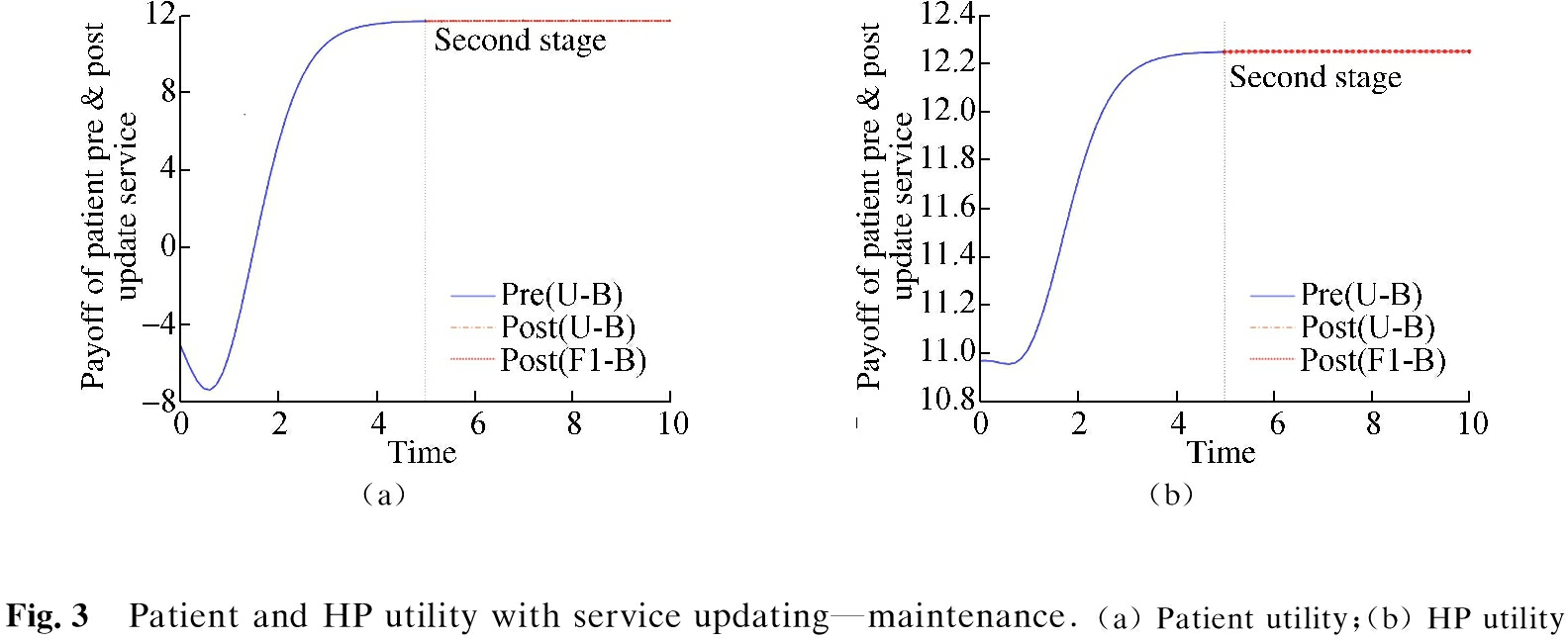
When HP and patient information quality are in the medium level, the payoffs for HPs and patients in the first period are U and B, and then the HP-oriented changes the payoff type to F1. Fig.3 shows the situation in which both users have reached an evolutionary equilibrium in the first stage, and the service update cannot achieve utility enhancement. That is, when patients and HPs have reached equilibrium in the early stage of platform operation, HIE is neither necessary nor improves user utility through price adjustment or service upgrade.
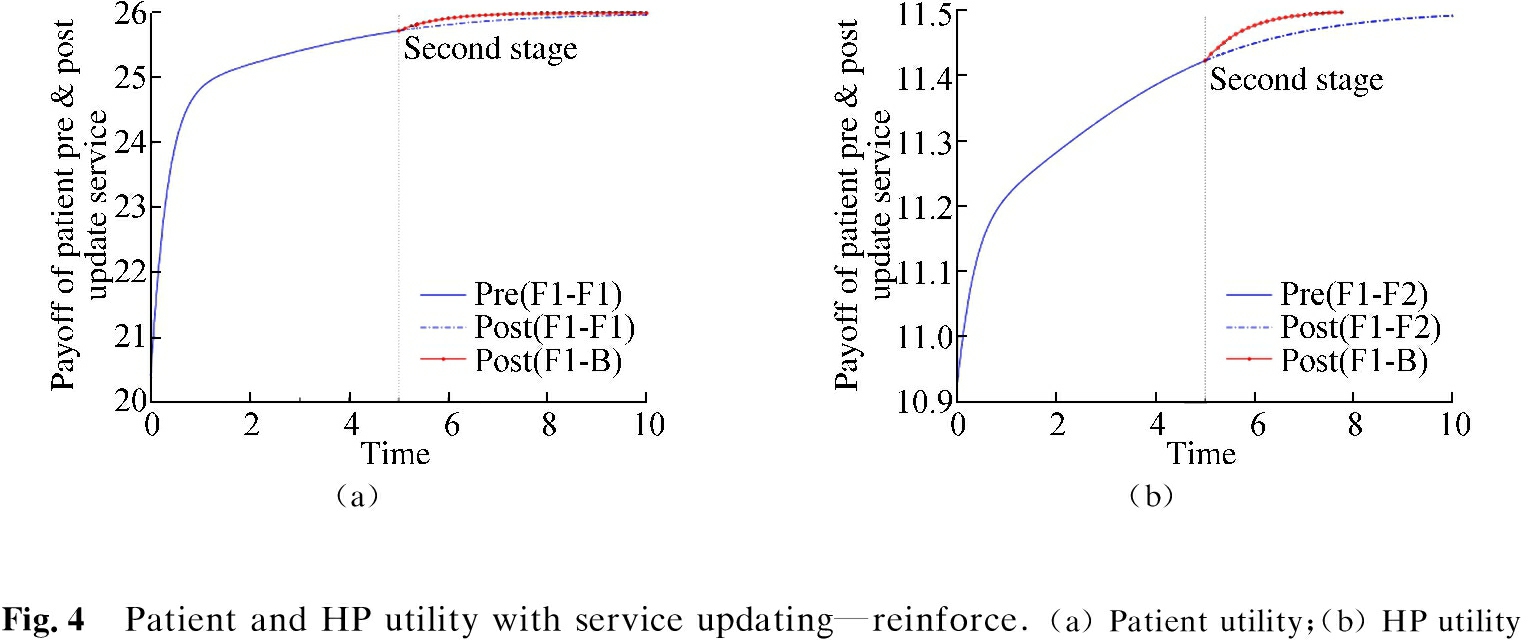
When HP information quality is low and patient information quality is medium, the payoff for HPs and patients in the first period is F1, and then the patient-oriented service updating changes the payoff to B. Fig.4 illustrates that utility improvements for HIE platform users can be achieved by providing HP-oriented service upgrades. When the utility of both parties increases with time druing the first stage, the HP-oriented service upgrade of HIE can improve the equilibrium utility of users of both parties in the second stage.
When HP information quality is low and patient information quality is medium, the patient payoffs are F2 and B, and then HP-oriented service updating changes the payoff from U to F1. Fig.5 indicates the effect of patient-oriented service updating on HIE user utility. In the first stage, the diminishing utility of users indicates that platform sustainability is weak; then, the patient-oriented service upgrade can help enhance the sustainability of the platform to improve the user utility.

In sum, patient service updating is more recommended than HP-oriented service updating to improve HIE sustainability. The HP-oriented service upgrade helps improve the equilibrium utility of both sides without prolonging the time for ESS. Patient-oriented service upgrade helps turn the tide and improve platform sustainability and even speed up the ESS process.
4 Conclusions
1) This study adopts evolutionary game theory to study the dynamic cooperation process between patients and HPs on the HIE service platform. We provide a novel insight to manage HIE sustainability, and the numerical simulation analysis is performed.
2) Information quality and initial user participation affect HIE sustainability. The high initial participation fraction and high data quality of HPs and patients in the HIE platform are essential factors for realizing the SMC mode, which evolves to HVC. The information service upgrade helps to improve the sustainability of the HIE platform and systematically enhance the utility of participants. Patient service updating is more recommended than HP-oriented service updating because of its performance and time efficiency.
3) To improve the operational maturity and sustainability of the HIE platform, managers can invest more in patient information collection to improve the quality of patient data or create patient-friendly incentives to upgrade services for shaping HVC.
[1]McColl-Kennedy J R, Snyder H,Elg M, et al. The changing role of the health care customer: Review, synthesis and research agenda[J]. Journal of Service Management, 2017.DOI:10.1108/JOSM-01-2016-0018.
[2]Demirezen E M, Kumar S, Sen A. Sustainability of healthcare information exchanges: A game-theoretic approach[J]. Information Systems Research, 2016, 27(2): 240-258.DOI:10.1287/isre.2016.0626.
[3]Bodenheimer T. Coordinating care—a perilous journey through the health care system[J].North England Journal of Medicine,2008,358(10):1064-1071.DOI:10.1056/NEJMhpr0706165.
[4]Lee D H. Effects of key value co-creation elements in the healthcare system: Focusing on technology applications[J]. Service Business, 2019, 13(2): 389-417.DOI:10.1007/s11628-018-00388-9.
[5]Ezra M,Dave T.Telemedicine is exploding,but where is the ROI for health systems[EB/OL].(2020-08-04)[2021-01-31].https://www.hfma.org/topics/financial-sustainability/article/telemedicine-is-exploding-but-where-is-the-roi-for-health-syste.html.
[6]Nosratabadi S, Mosavi A, Shamshirband S, et al. Sustainable business models: A review[J]. Sustainability, 2019, 11(6): 1663.DOI:10.3390/su13137266.
[7]Chandrasekaran R, Sankaranarayanan B, Pendergrass J. Unfulfilled promises of health information exchange: What inhibits ambulatory clinics from electronically sharing health information? [J]. International Journal of Medical Informatics, 2021, 149: 104418.DOI:10.1016/j.ijmedinf.2021.104418.
[8]Iyengar K, Jain V K, Vaishya R. Pitfalls in telemedicine consultations in the era of COVID 19 and how to avoid them[J]. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 2020, 14(5): 797-799.DOI:10.1016/j.dsx.2020.06.007.
[9]Hosseini-Motlagh S M, Johari M, Zirakpourdehkordi R. Grain production management to reduce global warming potential under financial constraints and time value of money using evolutionary game theory[J]. International Journal of Production Research, 2020,59(17):5108-5129.DOI:10.1080/00207543.2020.1773562.
[10]Wang T, Li C, Yuan Y, et al. An evolutionary game approach for manufacturing service allocation management in cloud manufacturing[J].Computers & Industrial Engineering, 2019, 133: 231-240.DOI:10.1016/j.cie.2019.05.005.
[11]Babu S, Mohan U. An integrated approach to evaluating sustainability in supply chains using evolutionary game theory[J]. Computers & Operations Research, 2018, 89: 269-283.DOI:10.1016/j.cor.2017.01.008.
[12]El Attaoui A, Largo S, Jilbab A, et al. Wireless medical sensor network for blood pressure monitoring based on machine learning for real-time data classification[J]. Journal of Ambient Intelligence and Humanized Computing, 2021,12(9):8777-8792.DOI:10.1007/s12652-020-02660-1.
[13]Layman E J. Ethical issues and the electronic health record[J]. The Health Care Manager, 2020, 39(4): 150-161.DOI:10.1007/s10880-017-9537-4.
[14]Khuntia J, Mithas S, Agarwal R. How service offerings and operational maturity influence the viability of health information exchanges[J]. Production and Operations Management, 2017, 26(11): 1989-2005.DOI:10.1111/poms.12735.
[15]Rajapakshe T, Kumar S, Sen A, et al. Sustainability planning for healthcare information exchanges with supplier rebate program[J]. Operations Research, 2020, 68(3): 793-817.DOI:10.1287/opre.2019.1912.
[16]Eraker S A, Kirscht J P, Becker M H. Understanding and improving patient compliance[J]. Annals of Internal Medicine, 1984, 100(2): 258-268. DOI:10.7326/0003-4819-100-2-258.
[17]Adler-Milstein J, Raphael K, O′Malley T A, et al. Information sharing practices between US hospitals and skilled nursing facilities to support care transitions[J]. JAMA Network Open, 2021, 4(1): e2033980.DOI:10.1001/jamanetworkopen.2020.33980.
[18]Ayvaci M,Cavusoglu H,Kim Y,et al.Designing payment contracts for healthcare services to induce information sharing:The adoption and the value of health information exchanges (HIEs)[J].Management Information Systems Quarterly,2021,45(2):637-692.DOI:10.25300/MISQ/2021/14809.